A Hearing Aid is a device designed to improve hearing by making sound audible to a person with hearing loss. Hearing aids are classified as medical device in most countries, and regulated by the respective regulations.
Modern era hearing aids require configuration to match the hearing loss, physical features, and lifestyle of the wearer. The hearing aid is fitted to the most recent hearing test (Audiometry) and is programmed by frequency. This process called “fitting” can be performed by the user in simple cases, by a Doctor of Audiology, also called an Audiologist/Hearing Doctor.
A hearing aid trial is a process where an individual with hearing loss tries out hearing aids to assess their effectiveness and suitability. The trial typically lasts a few weeks to a few months, allowing the individual to experience the benefits and make adjustments before committing to a purchase.
1. Fitting: The hearing aids are programmed and fitted to the individual’s specific hearing needs.
2. Orientation: The individual receives instructions on using and caring for the hearing aids.
3. Follow-up appointments: Regular check-ins with the audiologist or hearing specialist to:
– Adjust settings as needed
– Address any concerns or issues
– Monitor progress and satisfaction
– Determine the effectiveness of the hearing aids in improving communication and quality of life
– Identify any issues or limitations with the hearing aids
– Make informed decisions about purchasing the hearing aids or exploring alternative options
A successful hearing aid trial can lead to:
– Improved communication and social interaction
– Enhanced overall satisfaction and quality of life
– Increased confidence in using hearing aids
– Speech understanding in noise/quiet/Group Conversation
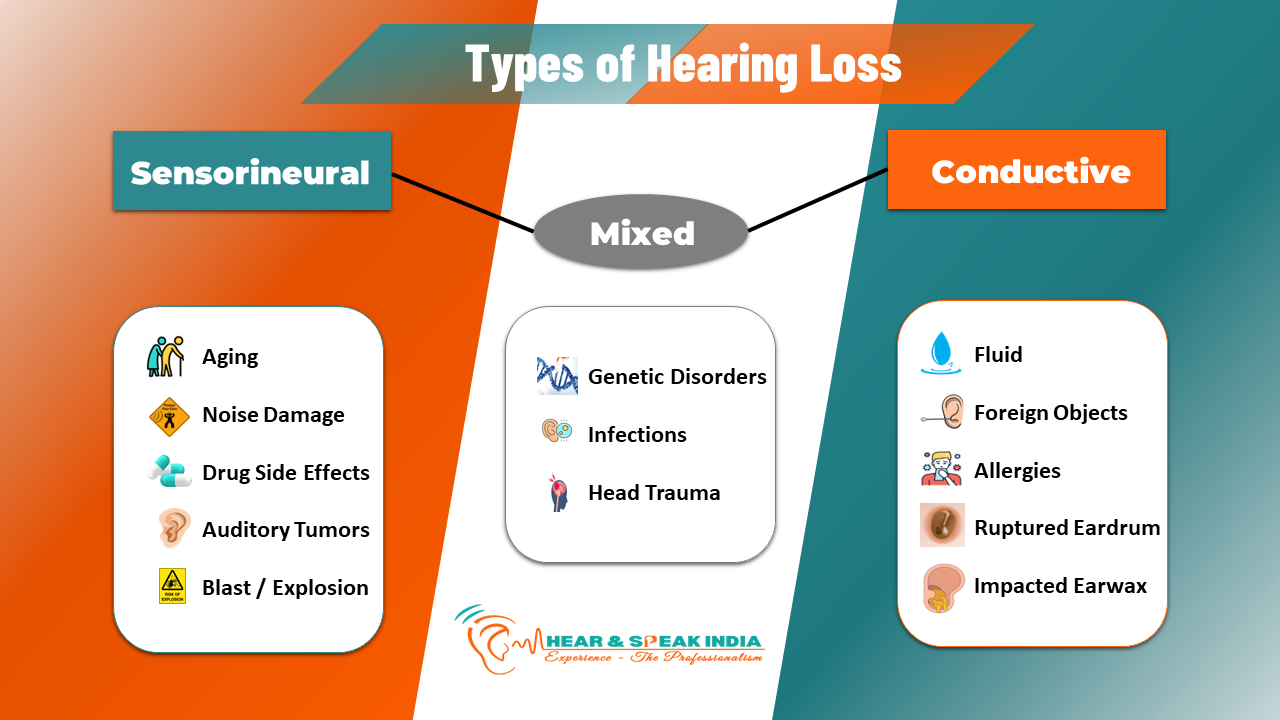
In this hearing loss, something keeps sound from passing through your outer ear (ear canal) or your middle ear.
This hearing loss happens when something damages your inner ear over time.
This happens when you have issues in your middle or outer ear (conductive hearing loss) and your inner ear (sensorineural hearing loss)
Audiologists are health care professionals who identify, assess and manage disorders of hearing, balance and other neural systems.
Audiologists earn a master’s degree in audiology from an accredited university along with Dissertation Paper for Course completion with 4 scientific paper.
Audiologists serve a fellowship or externship year and must pass boards to receive licensing and accreditation from Rehabilitation Council of India (RCI). Further, audiologists enroll in continuing education credits to continue practicing licensing.
Typically, audiologists achieve certification from the national association Rehabilitation Council of India (RCI).

The OAE test is a quick, painless, and non-invasive hearing test for babies. It measures the sounds produced by the inner ear in response to sound stimuli.
– Normal hearing
– Hearing loss (permanent or temporary)
– Middle ear problems (e.g., fluid or blockage)
Results are usually available immediately, and the test can be repeated if necessary.
Why OAE?– It’s a simple, painless test for babies
– It can detect hearing issues early, crucial for language development and intervention
– It’s a reliable indicator of inner ear function
The OAE test is usually part of a comprehensive newborn hearing screening program.
The BERA test is a non-invasive, objective hearing assessment that measures the brain’s response to sound. It’s used to:
1. Detect hearing loss, especially in newborns and young children
2. Assess the auditory nerve and brainstem function
3. Diagnose auditory neuropathy and other hearing disorders
– Other hearing disorders
The BERA test is:– Pain-free and non-invasive
– Quick (usually 45 minutes)
– Reliable and objective
– Essential for early detection and intervention in hearing loss
Note: The BERA test is often used in conjunction with other hearing tests, like OAE, to provide a comprehensive assessment.
Hearing test (PTA) used to identify hearing threshold levels of an individual, enabling determination of the degree, type and configuration of a hearing Loss and thus providing a basis for diagnosis and management.
Pure-tone audiometry is a subjective, behavioural measurement of a hearing threshold, as it relies on patient responses to pure tone. Therefore, pure-tone audiometry is only used on adults and children old enough to cooperate with the test procedure.
As with most clinical tests, standardized calibration of the test environment, the equipment and the stimuli is needed before testing proceeds (in reference to ISO, ANSI, or other standardization body).
Although pure-tone audiometry has many clinical benefits, it is not perfect at identifying all losses, such as ‘dead regions’ of the cochlea and neuropathies and monitor hearing loss, as well as to assess the effectiveness of hearing treatments type of Hearing loss.
Speech Audiometry is a type of hearing test that assesses an individual’s ability to understand speech in various environments. It evaluates how well the brain processes speech sounds, including:
1. Speech Recognition Threshold (SRT): The softest speech sound detectable.
2. Word Recognition Score (WRS): The ability to repeat words correctly.
3. Speech in Noise (SIN) testing: Evaluates speech understanding in background noise.
– Speech recognition in quiet and noisy environments
– Ability to understand speech with different accents or speaking styles
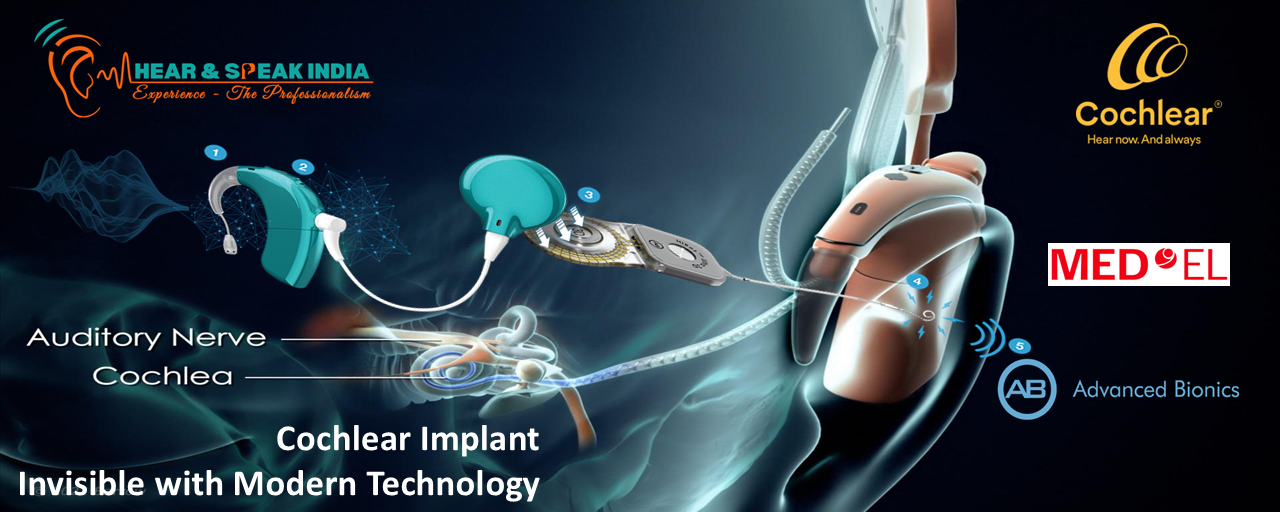
– Effectiveness of hearing aids or cochlear implants in improving speech understanding
Results help diagnose:– Hearing loss
– Auditory processing disorders
– Speech recognition difficulties
Speech Audiometry is essential – Evaluating hearing aid or cochlear implant effectiveness
– Assessing auditory rehabilitation progress
– Identifying communication difficulties in everyday situations
Tympanometry is a non-invasive test used to assess the function of the middle ear system, including the eardrum (tympanic membrane), ossicles (small bones), and Eustachian tube. It measures the movement and flexibility of the eardrum, as well as the Acoustic reflexes of the middle ear muscles.
Helps to Detect-
– Eardrum mobility and compliance
– Middle ear pressure
– Eustachian tube function
– Reflexes of the stapedius and tensor tympani muscles
Tympanometry results can help diagnose– Middle ear infections (otitis media)
– Eustachian tube dysfunction
– Eardrum perforations or scarring
– Ossicular damage or fixation
– Patulous Eustachian tube
The test is painless, quick, and provides valuable information for diagnosing and treating middle ear disorders.
The Tone Decay Test is a hearing assessment tool used to detect auditory fatigue or adaptation in the auditory nerve or brainstem. It measures how well the auditory system can sustain its response to a continuous tone.
Helps to differential diagnosis of
– Auditory nerve damage or dysfunction
– Brainstem lesions or disorders
– Auditory processing disorders
Tinnitus (“TIN-a-tus” or “Tin-EYE-tus”) is the medical term for the sensation of hearing sound in your ears or head when no external sound is present. In most cases, tinnitus is a subjective noise, meaning only the person experiencing it can hear it. Typically, people describe the sound as “ringing in the ears,” though others describe it as hissing, buzzing, whistling, roaring and even chirping. Tinnitus can be sporadic or constant, with volume ranging from subtle to debilitating.

Tinnitus is most often described as a ringing in the ears, even though no external sound is present. However, tinnitus can also cause other types of phantom noises in your ears, including:
Most people who have tinnitus have subjective tinnitus, or tinnitus that only you can hear. The noises of tinnitus may vary in pitch from a low roar to a high squeal, and you may hear it in one or both ears.
In rare cases, tinnitus can occur as a rhythmic pulsing or whooshing sound, often in time with your heartbeat. This is called pulsatile tinnitus. If you have pulsatile tinnitus, your doctor may be able to hear your tinnitus when he or she does an examination (objective tinnitus).
In many people, tinnitus is caused by one of the following:
Anyone can experience tinnitus, but these factors may increase your risk:
Tinnitus affects people differently. For some people, tinnitus can significantly affect quality of life. If you have tinnitus, you may also experience: